Increase in eosinophil cationic protein is one of the reasons for the cerebrovascular diseases and related neurological disorders
The main idea: an increased level of eosinophil cationic protein facilitates cerebral vascular spasms. The word «spasm» in this context means temporal blood vessels constriction, while the degree of constriction may vary significantly.
The material was prepared by a person without medical education after struggling with neurological disorders described in the article (see «About the author»). There may be some loss in translation, so if any question arises, please contact the author by e-mail mbrain16@outlook.com.
The main text of the article was written in 2017, supplemented in 2018-21.
Contents
- Abstract
- Possible symptoms
- Cerebral vascular spasms
— Trigger-factors
— Condition-factors - Neurotoxic effect of ECP
- Connection between increased ECP level and vascular spasms
- Reasons for increase in ECP
- Conclusion
- References
- Appendix: Additional versions and observations after writing the article (period of 2018-21)
- Collaborative research proposal
Version of apr.20: bacteria similar to rickettsia
About the author
Download PDF version
1. Abstract
Various cerebrovascular diseases and concomitant neurological disorders may be connected with an increased level of eosinophil cationic protein (ECP) in the blood.
ECP is a small protein released from eosinophils as a result of certain immune reactions. ECP increase is possible in case of different states connected with allergic reactions, bacterial infections, parasitic invasions, etc.
ECP is known to be a neurotoxin, but the author believes that the impact on the brain is not only the result of a direct neurotoxic effect, but also of a mediated effect – through cerebral vessels constriction (spasm). The author suggests that increased ECP level contributes to spasms of the brain vessels, leading to ischemia of separate parts of the brain and concomitant neurological disorders. The variety of neurologic manifestations in this case is connected with the fact that at different moments different parts of the brain may suffer from ischemia which result in focal neurological disorders. Despite the temporary nature of the disturbances, in the long term the condition probably may lead to encephalopathy as a result of neuron death and vessel wall thickening.
The mechanism of ECP influence on the vessels may include several factors (a detailed description is given in the main text of the article):
- change in permeability of cell membranes and disruption of key ions homeostasis (including Ca2+) in autonomic [vegetative] neurons and astrocytes, which results in a local uncontrolled discharge of neurotransmitter (noradrenaline), especially when the cervical spine and cervical nerves are affected;
- change in permeability of cell membranes and disruption of key ions homeostasis in vascular smooth muscle cells, which disturbs the mechanism of their constriction and relaxation especially under the influence of vasoactive substances;
- damage of the vessel wall, leading to dysfunction of vessels’ endothelium and discharge of vasoactive substances in case of direct (including «mechanical») influence on the vessels.
Disturbances are possible even in case of a moderate increase in ECP level (30-40 ng/ml with the norm of <24 ng/ml), without an increase in eosinophils and without Hypereosinophilic Syndrome (this is important in terms of extent of such diseases spreading). Similar influence may probably be produced by the ECP relatives, major basic protein (MBP) and especially eosinophil-derived neurotoxin (EDN).
Possible reasons of increase in ECP: inflammatory processes in intestines (as a result of small intestine bacterial overgrowth, sensitivity to gluten, liver and bile ducts diseases, etc.), parasitic invasions, allergic reactions, bacterial infections (for example, in the nasopharynx), etc.
Thus, if there are neurological disorders of unclear etiology, it may be reasonable to take an ECP assay. If increased values are found, the reason for the increase (primary disease) ought to be defined and treated first. Before ECP normalization, the afflicted person’s condition may be improved significantly by taking selective calcium channel blockers (for example, nimodipine) or α1-adrenoreceptor blockers, and by minimizing trigger-factors which launch the constriction mechanism.
The practical value of the article consists of the description of non-evident reasons for neurological disorders and cerebrovascular diseases, as well as the method of their timely detection (that is control of eosinophil cationic protein levels).
The scientific value consists of a description of the mechanism of mediated influence of the eosinophil cationic protein on the brain, which differs from the direct neurotoxic effect described in medical studies. The described mechanism may play an important role in the appearance of a number of cerebrovascular diseases.
Keywords
Eosinophil cationic protein, vascular spasms, focal neurological disorders, cerebrovascular disease, transient ischemic attack, stroke, encephalopathy, vascular dementia, gut-brain connection, intestinal inflammation, gluten enteropathy, parasitic invasion.
Limitations
The material was prepared by a person without medical education, so there may be some inaccurate points in the article. The author will be glad about any comments and remarks, but at the same time calls to focus primary attention on the key idea of the article rather than specific details.
The author does not have a sufficient base for statistically reliable conclusions at his disposal. The conclusions are based on a number of scientific articles (mostly about ECP) and on personal observations and experiments on the medical assays background.
In Western practices, one may find articles that are based on a description of one notable case («case reports»). The purpose of these articles is not to prove something, but to draw the attention of the medical and scientific community to notable observations. This is the purpose of this article as well.
An additional limitation is imposed by the fact that the author was limited by analyses accessible in Russian commercial laboratories. For example, other ECP-related proteins, eosinophil-derived neurotoxin (EDN) and major basic protein (MBP), may play an important role, but the author had no possibility to do these analyses. Similarly, sensitivity to gluten is determined on the basis of 6 analyses in the laboratories accessible for the author, while Western practice uses a much larger number of tests.
2. Possible symptoms
During the study of the topic the author used observed symptoms as a basis, so the article starts with their description. Symptoms varied significantly and changed with the course of a disease. During the first year of the disease (2011) it was difficult to clearly define the symptoms — on rare days there was a sense of overall mental dullness (like in case of fever or hangover) and sometimes a feeling of an increased intracranial pressure. Symptoms became more pronounces with a course of time, and at the same time more varied and clearly defined — that is, focal neurological signs were observed. Such symptoms were transient (from several minutes to several hours) and reversible. The symptoms could be observed independently from each other. Frequency, variety and severity of the symptoms increased with the course of time, and the author believes that in worst periods (end of 2014) there were signs of the transient ischemic attack verging on ischemic stroke.
The list of possible symptoms is given below (they are grouped for convenience of reading, though it’s probably possible to group them by the localization of the disturbances):
Mental abilities
- Considerable problems in performing simple mental work which does not seem complicated at other times;
- considerable deterioration of memory, complications while attempting to recall simple things (for example, date of birth);
- inability to focus attention and concentrate;
- decrease in clarity of mind and overall mental dullness.
Speech
- decrease in speech clarity, unintelligible speech, inability to pronounce some words;
- incoherence, irrationality of speech, difficulties with thoughts formulation;
- substitution of words, inability to remember or choose the proper word;
- difficulties with understanding other people’s speech.
General condition
- clouded consciousness (similar to the state during high fever, condition on the verge of fainting);
- mood inadequate to the situation (risibility, euphoria, absence of emotions, etc.).
Other
- pain in the eyes (often in one eye), temporary impairment of vision, diplopia, defocusing of vision;
- impairment of hearing (often on one side), tinnitus;
- change in face mimics (masklike face, lowered edges of lips);
- negligence, unsteady gait;
- changed handwriting, omission of letters in words, frequent mistakes during typing.
Possible concomitant symptoms
- feeling of tension in the occipital lobe of the head;
- eye dryness, eye redness;
- mydriasis;
- allergic signs of unclear etiology (dermatitis, itchiness, rhinitis, etc.);
- very frequent yawning, feeling of being unable to inhale fully.
As previously mentioned, the symptoms were observed independently from each other, i.e. it was possible that the author could easily perform mental work but had difficulties with explaining it in an intelligible way. The state could be «tested» by doing simple operations, such as multiplication in mind, telling tongue twisters, formulating a monologue on a free topic, etc. At different time points difficulties with different actions occurred.
The severity of symptoms may also vary, they may be barely noticeable (even from the patient’s point of view) or they may considerably influence behavior and work capacity.
3. Cerebral vascular spasms
The author believes now that the described neurological disorders were caused by ischemia of separate parts of the brain as a result of vessels constriction (spasm). This conjecture was initially based on the results of funduscopy (it was said in the conclusion that the vessels of the eye ground are slightly narrowed) and a sense of the localization of disorder — sense that some definite brain areas suffer from ischemia (it could be felt despite of the absence of pain). At the same time MRI, angiography and other studies did not reveal any organic pathology. The important fact confirming the version of vessel spasms was a remarkable improvement after taking selective calcium channel blocker — nimodipine.
Studying vessels’ spasms origin, it’s seems reasonable to divide a cause of their emergence into two parts:
- trigger-factors — factors that trigger the mechanism of spasm (that is, leading to immediate spasm);
- condition-factors — factors that enable the launching of the spasm mechanism even when minor trigger-factors occur. Not all people suffer from vascular spasms, whereas everybody is exposed to trigger-factors, so it is the presence of condition-factors that may differentiate an ill person from a healthy one.
Trigger-factors
Trigger factors may be numerous and diverse. They may include turning of the head, working with a low tilt of the head (for example, while reading from paper or during work with a low located monitor), sleeping on a too high/low pillow, forced inconvenient position, harsh riding, uncomfortable clothes and so on.
A considerable part of these factors is connected with the neck (in one way or another), in particular — with vertebral arteries and/or cervical nerves. The cervical nerves braid vertebral arteries and innervate the brain vessels which make up the basin of vertebral arteries [Малыхин, 2007]. It was described in [Попелянский] that impact on the cervical nerves (for instance as a result of an injury or spine diseases) may lead to a reflectory spasm of vessels («cervical nerves syndrome»).
In the Soviet and Russian practice, a connection between neurological disorders and the state of the spine is considered by such a branch of neurology as vertebroneurology promoted by prof. Popelyansky. However, vertebroneurology is often being criticized, and it is thought to be in crisis now, partly due to the fact that practical observations do not fully conform to the theoretical basis [Ахмадов, 2012]. Discrepancies in vertebroneurology were described by a follower of prof. Popelyansky – prof. Veselovsky, who also noted «absence of parallels between the degree of expression of clinical signs and X-ray changes in case of dystrophic damage of the spine» [Ахмадов, 2012].
In case of the author, problems with the cervical spine do not completely explain the observed symptoms either. Firstly, personal observations show that triggers are sometimes the events not connected with the cervical spine, for example, eating a lot of sweets (probably, due to a vasoconstrictive effect of insulin), smoking (vasoconstrictive effect of nicotine) or bright light. Secondly, at certain moments (especially at the end of 2014), spasms were caused by as little as brushing teeth or a slightest turn of the head, while in other periods there were no spasms for weeks with the same trigger-factors. At the same time, no considerable changes in the state of the cervical spine were observed.
Thus, the author believes that these factors play a role of a trigger, but it’s only a part of a problem, while vascular spasms occur only under certain conditions.
Condition-factors
One of the first directions of investigating condition-factors was the study of the renin-angiotensin system. It was assumed that its dysfunction may be a predisposing factor for vascular spasms. Specifically, it was supposed that spasms are caused by the dysfunction of vascular endothelium, which could have meant that the impact on the vessels (in case of trigger-factors) made the vessel wall produce vasoactive substances (endothelin and angiotensin converting enzyme), leading to the spasm further along the blood vessels.
The author considered vasculitis connected with some autoimmune processes as one of the possible reasons for endothelial dysfunction. At the same time, a connection was observed between the strengthening of neurological disorders and different allergic signs of unclear etiology (dermatitis, eruption on the head skin, formation of crusts in the nasal cavity, etc.). All that led to the conjecture of an immune-allergic nature of the disease. As a result the author performed (among others) eosinophil cationic protein assay which turned out to be elevated (fluctuated within range of 24-50 ng/ml with the norm of <24 ng/ml).
At this moment the author suggests that the mere fact of ECP increase is the predisposing factor (i.e. condition-factor) which makes cerebral vascular spasms possible even as a result of minor influence on the vessels and/or cervical nerves.
4. Neurotoxic effect of ECP
Eosinophilic cationic protein is a small protein released from eosinophils as a result of certain immune reactions. ECP is known to be a neurotoxin [Soroka, 1995; Fredens, 1982; Navarro et al., 2010]. The initial information of eosinophils’ neurotoxicity refers to the 1930s when the «Gordon’s phenomenon» was described — that is neurological disorders in rabbits after injection of lymph nodes suspension from a patient with Hodging’s disease. This effect was associated with the presence of eosinophils in the suspension. It was shown later that an ECP injection also leads to the Gordon’s phenomenon [Fredens, 1982].
By now, the cases of rapid development of dementia and early strokes in people with hypereosinophilic syndrome have been described [Briania et al., 2001; Kaplan, 2011; Nallegowda et al., 2003; Weaver, 1988]. Despite this, the mechanism of neurotoxic effect of ECP still has not been fully investigated.
The study [Navarro et al., 2010] gives the following conclusions following a number of experiments:
- ECP binds to the cell membrane, changing its permeability and altering the internal cell balance of key ions, affecting cell functioning. This refers to neurons as well as other kinds of cells [Navarro et al., 2007].
- ECP launches the mechanism of cell apoptosis (that is, the mechanism of «normal», «programmed» death).
- In the experiments, ECP leads to death of both neurons and astrocytes, with direct dependence of cells survival on ECP concentration.
- High ECP concentrations lead to a sharp upsurge in concentration of calcium ions inside the neuron/astrocyte.
The statement about the change in the intracellular balance of ions is especially important in the context of discussing the spasms of the cerebral vessels.
5. Connection between increased ECP level and vascular spasms
The direct neurotoxic effect of ECP described in the medical studies does not fully explain the symptoms observed by the author. According to the author’s observations, the main role in neurological disorders may be played exactly by the spasms of cerebral vessels which, in turn, may be also connected with an increased ECP level. Of course, the author has no means to investigate comprehensively the EСP impact on the vessels, but several mechanisms are likely to be involved here:
- Change in permeability of cell membrane and disruption of key ions homeostasis including Ca2+ (according to [Navarro et al., 2007, 2010]) in vegetative neurons, which increases their excitability and leads to a local uncontrolled discharge of the neurotransmitter — noradrenaline, which has a strong vasoconstrictive effect.
This version matches the «cervical nerves syndrome» in the best way, that is, the increased ECP level makes cervical nerves more excitable and leads to a discharge of vasoconstrictors in the issue of even a slight impact on the cervical spine.
This version describes well the author’s personal observations, according to which the probability of spasm depends on the current ECP level. With normal ECP level spasm practically does not occur (regardless of the trigger-factors), with high ECP levels it occurs even under slightest trigger-factors. Also, the spasm may occur in different parts of the brain, probably depending on where noradrenaline was discharged.
Quite possibly this effect of a local uncontrolled neurotransmitter emission may explain muscular spasms as well. There are at least two notable cases showing the connection of ECP and myalgia: toxic oil syndrome outbreak in 1981 in Spain and eosinophilia–myalgia syndrome outbreak in 1989 in the US.
- Change in permeability of cell membrane and disruption of key ions homeostasis (according to [Navarro et al., 2007, 2010]) in vascular smooth muscle cells, which disturbs the mechanism of their constriction and relaxation especially under the influence of vasoactive substances. A similar mechanism was described with regards to bronchi in [Madison et al., 2000]. This version is supported by the presence of trigger-factors not connected with the cervical spine.
- Damage of the vessel wall by the ECP, leading to the dysfunction of vessels’ endothelium. In case of endothelial dysfunction, the «mechanic» impact on vessels may cause the release of vasoconstrictors and distribution of spasm further along the vessels. The impact of ECP on the vessels was mentioned in [Weaver, 1988; Soroka, 1995]. However, in [Weaver, 1988] it is assumed that the impairment of the vessel wall leads to a thrombosis and to embolic brain infarction as a consequence. The author of this article suggests another cause of ischemia – vasospasms themselves (with or without thrombosis). This is an important difference, as it assumes use of the other therapeutic means (calcium channels blocking agents and α1-adrenoceptor blocking agents).
This version is supported by the fact of gradual aggravation of symptoms (gradual endothelium damage is possible). However, this version is contested by the fact that the spasm occurs in different parts of the brain. If it was the main reason, vasoconstrictors would be produced in the same place of vertebral artery and influence the same brain parts after turning the head. Furthermore, it was noted that the most pronounced spasmolytic effect was produced by calcium channels blocking agents and α1-adrenoreceptor blocking agents, while taking angiotensin-converting enzyme inhibitors and angiotensin-II receptor antagonists did not give any noticeable result (so it supposed to be less probable that the problem is connected with a discharge of angiotensin converting enzyme).
- Disruption of key ions homeostasis (according to [Navarro et al., 2007, 2010]) in astrocytes, which may also produce vasoactive substances. This mechanism is supported by general deterioration of state when ECP is particularly high, even in absence of evident trigger factors and without sense of the localization of the disorder.
The same influence may probably be exerted by ECP-relative proteins — major basic protein (MBP) and especially eosinophil-derived neurotoxin (EDN), which has the properties similar to a large degree to properties of ECP [Gleich G. et al., 1986; Navarro S. et al., 2010].
Regardless of which mechanism plays the main role here, all of them may facilitate the occurrence of the cerebral vascular spasms. Also, despite the transitory nature of spasms, it seems quite natural that they may lead to encephalopathy in the long-term due to neuron death and vessel wall thickening.
6. Reasons for increase in ECP and additional observations
*Despite the described common mechanism of the relationship between high ECP levels and neurological symptoms, the prime cause of an increase in ECP may be very different. This section is less scientific, contains fewer references to literature and more personal observations, the information may be updated and expanded*
The reasons for increase in ECP may be quite individual, so finding the only reason, relevant for all the afflicted persons, is not the purpose of this section. An increase in ECP may result from a multitude of factors, and unfortunately they are not always evident.
The following reasons for an increase in ECP are enumerated in literature/on the Internet most often:
- parasitic invasions;
- allergic reactions;
- bacterial infections;
- bronchial asthma;
- autoimmune processes.
Less often ulcers and intestinal inflammation are added to the list.
Let’s consider the main reasons in detail on the author’s experience. While reading, it may be noticed that many reasons for ECP increase (primary diseases) are already associated with different neurological disorders in the literature (despite the fact that increase in ECP is not mentioned in that cases). That is, increased ECP level unites different diseases which may result in neurological disorders.
Parasitic invasions
Parasitic invasion was the first version to investigate (in the case of the author it was not confirmed later on). ECP is toxic for parasites [Soroka, 1995] and its level increases with most parasitic invasions. It’s interesting to note that both leading and ordinary employees of the Martsinkovsky Parasitology Center (Moscow) were not surprised at a possible connection between neurological disorders and parasites. Neurological disorders caused by invasions are quite well-known and evident for parasitologists. It is important that this effect is produced not only by rare parasites, located right in the brain, but also all of the most widespread kinds. The concomitant neurological disorders are usually connected with their toxic influence on the body.
Thus, the first thing that may be investigated in case of an increased ECP (especially in children) is the presence of the most widespread parasites.
Allergic reactions
The author’s next version was hidden allergic reaction. The main allergens (respiratory and food panels) were tested, but the result did not give any reason to talk about allergy.
However, it was found out later that food panels do not allow to precisely define one of the widespread food allergies, sensitivity to gluten. Sensitivity to gluten is determined by a whole number of specific tests. Russian laboratories use about 6 tests, while there are about 24 of them in the Western practice (CYREX array 3). Probably this is the reason why gluten-sensitive enteropathy is diagnosed much more frequently in the western countries. Besides, in accordance with present day knowledge of gluten-sensitive enteropathy, this disease is no longer considered to be rare, and distribution of its hidden forms may achieve 1:100 [Парфенов, 2013], and according to some data — 1:3 [Perlmutter, 2013 / Перлмуттер, 2014]. Also, hidden forms of gluten-sensitive enteropathy often disguise as other diseases.
It turned out that the connection between sensitivity to gluten and neurological disorders had been already described, for example, in [Perlmutter, 2013 / Перлмуттер, 2014]. However, in [Perlmutter, 2013 / Перлмуттер, 2014] another mechanism of influencing the brain is described, i.e. without participation of ECP or vascular spasms.
Thus, in case of increased ECP level it may be also reasonable to take gluten sensitivity assays and, if necessary, sensitivity to other allergens (food and respiratory panels).
The question of whether the author is sensitive to gluten remains open. Five out of six tests are within reference values, and one is permanently increased (deamidated gliadin peptide antibodies, IgA). However, a biopsy did not confirm gluten-sensitive enteropathy, and the results of genetic studies also testify to its low probability. Gluten-free diet did not influence dynamics of ECP and deamidated gliadin peptide antibodies, though there are notable details described in the section «Additional comments».
Intestines inflammation (as a result of dysbacteriosis)
At the same time, a biopsy revealed inflammation of intestines (chronic duodenitis and colitis), supposedly of a bacterial nature (tests showed the development of opportunistic pathogenic and pathogenic microflora). Inflammation of intestines may also lead to increased ECP, and this was the author’s main version [as of 2017, at the time of writing the main text of the article] regarding the reason for ECP increase in the case of the author.
The following observations may be provided here:
— the author observed the longest remission period in the middle of 2014 (complete absence of neurologic disorders). At that moment, the author had no version about spasms or ECP, but it was noted that it had happened after a course of antibiotics (in connection with another disease);
— at the end of 2014, the author experienced a period of the most frequent, severe and continuous neurological disorders. Supposedly, after treatment with antibiotics in the middle of the year, the intestinal microflora was not completely restored, whereas a shortage of bifidobacterium and lactobacillus leads to the development of pathogenic microflora;
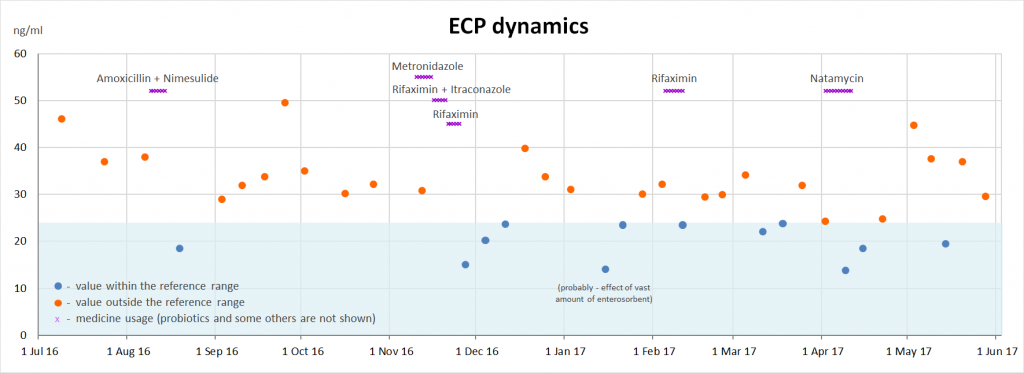
— in August of 2016, after treatment of another disease with antibiotics, ECP fell notably, but it restored over the following weeks (see the diagram below);
— in November of 2016, after duodenitis and colitis were diagnosed, treatment with antibiotics also resulted in falling ECP, but its level also restored over the following weeks;
— in April of 2017, taking Natamycin antimycotic agent (against Candida fungi whose development was discovered in dysbacteriosis analysis), which is active only in intestines, also resulted in a sharp decrease in ECP. However, it is possible that the decrease was connected not so much with elimination of Candida fungi but more with ECP withdrawal from the intestines as a result of Natamycin’s side effects; either way, the connection between ECP and intestines seems to be quite noticeable.
Thus, in case of increased ECP level it may be also reasonable to take dysbacteriosis assay (it worth be noted that in Western practice a term «(Small) Intestinal Bacterial Overgrowth» is used, which underlines the proliferation of pathogenic microorganisms in (small) intestine). If development of opportunistic pathogenic and pathogenic microflora is found, it’s reasonable to consult a gastroenterologist first. Before the microflora balance is restored, one can reduce the influence of ECP (and endotoxins associated with development of pathogenic microflora) by taking enterosorbents (for example, polymethylsiloxane polyhydrate). Also one need to keep in mind that the use of antibiotics requires complete recovering of microflora in the intestines and ensuring its state even in absence of complaints about GIT functioning.
It was found later that the connection of intestinal microflora with the brain had been also described [see literature by keywords «gut-brain axis», for example, Perlmutter, 2015]. But again, another mechanism of connection with the brain (without involvement of ECP and vascular spasms) is described.
Intestines inflammation (as a result of gastrointestinal tract organs disease)
At the same time, development of pathogenic microflora may only result from intestinal inflammation rather than cause it. Another possible reason of intestinal inflammation is the diseases of GIT organs, including biliary tracts and liver. It is noticeable that there is a separate term which connects brain disorders with liver diseases, hepatic encephalopathy. The concomitant neurologic disorders are also related to increased level of toxic substances in the blood. Therefore, it’s reasonable to take the relevant tests as well (ALAT, ASAT, Gamma GT, Bilirubin).
The author’s assays listed above are also within the normal range. The only relevant analysis outside reference values is bile acids.
Even though the author hasn’t found out the reason for intestinal inflammation, the dependence of ECP level on the state of the intestines seems quite evident (in the case of the author).
Other reasons
Other possible reasons for increased ECP:
- other gastrointestinal tract diseases (including intestinal ulcer);
- other bacterial infections (e.g. in nasopharynx);
- other allergic reactions;
- bronchial asthma;
- autoimmune diseases.
As the reasons are quite individual, additional hypotheses probably should be based on the afflicted person’s anamnesis.
Additional comments
* The information may be updated and expanded *
- Eosinophils were normal over the whole period of observations. ECP ranged within 24-50 ng/ml (with the normal value of <24 ng/ml). That is, the described case is not one of the quite rare hypereosinophilic syndromes. This is important in terms of extent of such diseases spreading.
- During practically the whole period of observations, the level of uric acid was increased (and it fell temporarily after duodenitis and colitis treatment). It’s interesting to note that there is information about the protective influence of uric acid in case of brain ischemia [Mattson M. et al., 2000].
- Of all blood assays (a very large list) only consistent increase in ECP, uric acid and deamidated gliadin peptide antibodies IgA were observed. The liver biochemistry samples have normal values (except for biliary acids). The thyroid gland is functioning normally.
- Dynamics of deamidated gliadin peptide antibodies IgA was not fully explained by the diet. The result could be quite low with consumption of gluten-containing products and quite high when a diet was followed [In 2019 there appeared a reason to believe that the results of these tests were mistake of one laboratory]. Probably sensitivity to gluten may also be connected with the state of intestinal microflora [Barcik W. et al., 2016; Caminero A. et al., 2015].
- The results of dysbacteriosis test were unstable in time and changed significantly even over one week. However, it was noticed that a deterioration of state and increase in ECP was possible without excessive growth of gram-negative bacteria. This fact supports the idea that the impact of intestinal microflora on the brain is connected not only with lipopolysaccharides (which result from the decay of gram-negative bacteria).
- Even though the author hasn’t achieved stable lowering of ECP yet, the overall state has been radically improved due to treatment with nimodipine (Nimotop, BAYER), control of trigger-factors and diet correction. It is quite possible that the average level of ECP as for the end of 2014 (when the most severe symptoms were observed) was significantly higher, but unfortunately it cannot be proved now.
7. Conclusion
Thus, on the one hand, an increase in ECP may play a key role in the development of a number of cerebrovascular diseases and concomitant neurological disorders, and on the other hand — an increase in ECP unites a number of diseases that are accompanied by neurological symptoms. That means that regardless of the reason for the ECP increase, which may be quite individual, the ECP assay could be a universal diagnostic mean which may be widely used in neurology to identify the problems predisposing to brain diseases in a timely manner.
It was noted in [Угрюмов] that the reason for chronic neurodegenerative diseases remains unknown in the majority of cases. The author of this article hopes that the influence of ECP will help to explain the whole range of cerebrovascular diseases and prevent their development in a large number of people.
Proposed work scheme
If there are uncertain neurological complaints, reduced mental ability, different neurological disorders of unclear etiology, the patient ought to take the ECP assay. In case of increased ECP level, the reason for the increase (primary disease) ought to be defined and treated first. While the symptoms remain, the patient’s state may be considerably improved:
- by taking selective calcium channel blocking agents (nimodipine); someone may benefit from α1-adrenoreceptor blocking agents (it should be borne in mind that some α1-adrenoceptor blocking agents, being the derivatives of ergot alkaloids (including nicergoline), are no longer recommended in Europe because of possible deferred side effects [EMA, 2013]);
- by defining and minimization of trigger-factors (for example, sleeping on the back, on a low orthopedic pillow, avoidance of sharp turns/bends of the head, quitting smoking, etc.);
- if necessary (depending on the supposed reason) — by taking anti-inflammatory agents, antihistaminic agents to reduce the degree of sensibilization, enterosorbents to reduce ECP and endotoxins in the intestines. Probably positive effect may also be produced by ginkgo biloba (due to blood viscosity reduction).
Furthermore, considering the chronic and often hidden nature of neurodegenerative diseases, the author believes that ECP assay is worth being included in medical checkup programs for control even in absence of complaints.
———
Any comments and remarks may be sent to mbrain16@outlook.com.
8. References
- Alfadda A., Storr M., Shaffer E., Eosinophilic colitis: epidemiology, clinical features, and current management. Therapeutic Advances in Gastroenterology, (2010) 4(5) 301-309
- Barcik W., Untersmayr E., Pali-Scholl I., O’Mahony L., Frei R., Influence of microbiome and diet on immune responses in food allergy models, DDMOD-428, 2016
- Briania C., Baracchinia C., Zanetteb G., Zanussob G., Carolloc C. and Monacob S., Rapidly progressive dementia in hypereosinophilic syndrome. European Journal of Neurology 2001, 8: 279-280
- Bystrom J., Amin K., Bishop-Bailey D., Analysing the eosinophil cationic protein — a clue to the function of the eosinophil granulocyte. Bystrom et al. Respiratory Research 2011, 12:10
- Caminero A., Nistal E., Differences in gluten metabolism among healthy volunteers, coeliac disease patients and first-degree relatives. British Journal of Nutrition (2015), 114, 1157–1167
- European Medicines Agency (EMA), New restrictions on use of medicines containing ergot derivatives, press release 28.06.2013
- Fredens K., Dahl R., Venge P., The Gordon phenomenon induced by the eosinophil cationic protein and eosinophil protein X. J Allergy Clin Immunol 1982, 70(5):361-366.
- Gleich G., Loegering D., Bell M., Checkel J., Ackerman S., McKean D., Biochemical and functional similarities between human EDN and ECP. Proc. Natl. Acad. Sci. USA Vol. 83, pp. 3146-3150, 1986
- Kaplan P., Central Nervous System Problems With Eosinophilia. Arch Neurol / Vol 68 (No 12), dec.2011
- Kazuko Shichijo, Kazuya Makiyama et al., Antibody to eosinophil cationic protein suppresses dextran sulfate sodium-induced colitis in rats. World Journal of Gastroenterology 2005;11(29):4505-4510
- Madison M., Schramm C., Cationic Proteins and Bronchial Hyperresponsiveness. American Journal of Respiratory Cell and Molecular Biology Vol. 22 2000
- Mattson M., Culmsee C., Zai Fang Yu, Apoptotic and antiapoptotic mechanisms in stroke. Cell Tissue Res (2000) 301:173–187
- Nallegowda M., Singh U., Handa G., Arora B., Idiopathic Hypereosinophilic Syndrome with Stroke in Young: A Case Report. IJPMR 14, April 2003; 24-26
- Navarro S., Aleu J., Jimenez M., Boix E., Cuchillo C. M., Nogues M. V., The cytotoxicity of eosinophil cationic protein/ribonuclease 3 on eukaryotic cell lines takes place through its aggregation on the cell membrane. Cell. Mol. Life Sci. 65 (2008) 324 – 337
- Navarro S., Boix E., Cuchillo C., Nogués V., Eosinophil-induced neurotoxicity: The role of eosinophil cationic protein/RNase 3. Journal of Neuroimmunology 227 (2010) 60–70
- Smaili S., Hirata H. et al., Calcium and cell death signaling in neurodegeneration and aging. An Acad Bras Cienc (2009) 81 (3)
- Stetka B., Perlmutter D., Dementia: Is Gluten the Culprit? Medscape. Jan 21, 2014.
- Vivian A., Salazar M., Exploring The Mechanism of Action of Human Antimicrobial Ribonucleases. Barcelona, 2015
- Weaver D.F., Heffernan L.P., Purdy R.A., Ing V.W., Eosinophil-induced neurotoxicity: Axonal neuropathy, cerebral infarction and dementia. Neurology 1988;38:144-146
- Wojda U., Salinska E. and Kuznicki J., Calcium Ions in Neuronal Degeneration. IUBMB Life, 60(9): 575–590, September 2008
- Yamasaki K., Makiyama K., Eosinophil Cationic Protein (ECP) in Ulcerative Colitis. Acta Med. Nagasaki 39: 67-71
- Ахмадов Т.З., Существует ли кризис в вертеброневрологии (организационные и методологические аспекты изучения проблемы остеохондроза позвоночника), Чеченский государственный университет, 2012
- Малыхин А.В., Вегетативные пароксизмальные состояния и терморегуляция организма
- Парфенов А.И., Глютенчувствительная целиакия – мультидисциплинарная патология человека. Верхневолжский медицинский журнал, 2013 — т.11, вып. 2.
- Перлмуттер Д., Еда и мозг (перевод с английского). Изд. «Манн, Иванов и Фербер», 2014
Translation of: Perlmutter D., Loberg K., Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar — Your Brain’s Silent Killers, 2013 - Перлмуттер Д., Лоберг К., Кишечник и мозг (перевод с английского). Изд. «Манн, Иванов и Фербер», 2017
Translation of: Perlmutter D., Brain Maker: The Power of Gut Microbes to Heal and Protect Your Brain–for Life, 2015 - Попелянский Я.Ю., Ортопедическая неврология (вертеброневрология), «МЕДпресс-информ», издание 2011
- Сорока Н.Ф., Савченко М.А., Современные представления о роли эозинофолов в организме и гиперэозинофильных синдромах. Журнал «Медицинские новости», №3, 1995
- Угрюмов М.В., Болезни мозга: как спасти нейроны (интервью), Harvard Business Review, 2014
Appendix: Additional versions and observations after writing the article (period of 2018-21)
*Please note that this section was translated by Google Translatе.*
Versions (regarding the root cause of violations, specifically from the author of the article)
- chronic tick-borne borreliosis (Lyme disease) — rejected [2018]; [2021: analyzes are contradictory]
- hypoacid stomach — rejected;
- Crohn’s disease — rejected;
- Whipple disease — rejected (biopsy not confirmed);
- violation of the metabolism of purines and pyrimidines — rejected;
- hypersensitivity to certain food additives (notably E211) — observations are mixed;
- «increased need» for nicotinic acid (vitamin B3) — observations are ambiguous;
- violation of amino acid metabolism is questionable;
- «increased intestinal permeability» — questionable;
- syphilis rejected.
- bacteria close to rickettsiae — questionable.
Observations
*Please note that this section was translated by Google Translatе.*
- C-reactive protein was normal throughout the observation period.
- May 18: After eating food with flavor enhancer E621 (monosodium glutamate), there is a feeling of fullness of the head, sometimes pain, sometimes an irritated / embittered state.
- Sep 18: After eating food with E211 (sodium benzoate) preservative, sometimes lethargy occurs. After an episode of a VERY strong inhibition (I was at lunch with a friend, the beginning of the conversation was normal, by the end of the lunch the reaction to the remarks in the conversation became with a delay of 1-2 seconds). To confirm the connection with E211, a urine test for organic acids was passed the next day. As a result, only Hippuric acid was increased (519.69 mmol / mol creat. With reference values 60.00 — 300.00), which is a derivative of benzoic acid.
- Mar.19: after using Biseptol, the ECP level dropped to zero (it recovered after a week). Possible side effects of the drug on the hematopoietic system (provided that there is no laboratory error).
- Apr 19: There was an episode of «bloody sweat» (hematidrosis). The episode was at night, with stress, fear, etc. (which, as they say, can be triggers of such a phenomenon) absolutely did not exist that day.
- Jun 19: It was noticed that with tension of the neck muscles and a feeling of spasm of the cervical arteries, a noticeable improvement occurs almost immediately (10 minutes) after eating very spicy food (chili pepper). Perhaps due to an irritating effect on the vagus nerve.
- Feb 21, Jul 21: one of the markers of Lyme disease (antibodies to antigens Osp, p31) was detected, in the absence of other markers (the final conclusion of the laboratory for Lyme disease is negative).
- Jun 21: For a long time (possibly several years) there are profuse rashes on the back and chest (acne). Previously, I did not draw a connection between rashes on the body and ECP, but in 2014, during the period of maximum severity of symptoms, I at least paid attention to rashes on the head (possibly a connection with rickettsia? See description below).
- Jul.21: increased immunoregulatory index (CD3 + CD4 + / CD3 + CD8 +), values around 3-3.5 (analyzes from Jul.16, May.19, Jul.21).
Version Apr 2020: bacteria similar to rickettsia
*Please note that this section was translated by Google Translatе.*
Description of the version in personal correspondence (unfortunately, now there is no time / energy to «refine» the text):
In short, a new version about my head. The most realistic, the most thorough, which fits almost all the various observations over many years. There are bacteria — rickettsia, so now I think it’s all because of them or the like. There are many types of them, one of them causes typhus (typhus is also many, caused by different bacteria). And one of the symptoms of typhoid is neurological disorders. But this does not sound concrete and not convincing, ok.
The main point is that this bacterium fits simultaneously in two lines of my theoretical thinking.
The first line is along the path of «vascular endothelial dysfunction», due to which the endothelium releases vasoconstrictors from any sneeze (such as turning the head ), which leads to spasm further up the bloodstream.
Rickettsia fits this theme by 1460%. To begin with, the wiki writes: «Rickettsiae have a tropism for vascular endothelial cells.» And elsewhere on the Internet: «In the human body, they are found in the cells that line the surface of blood vessels, which can cause problems with their inflammation, blockage or hemorrhage.»The second line (of my thoughts about the head) is along the path of «endotoxins» that are released during the decomposition of gram-negative bacteria. This line was connected with the fact that in some periods I had a constantly cloudy state, almost fainting and inadequate, like with a strong hangover, and this without any turning of my head. Therefore, I tested the theory of communication with the gastrointestinal tract, etc. — since «endotoxin aggression» is possible with all kinds of «bacterial overgrowth syndromes» in the gastrointestinal tract.
And lo and behold, this bacterium is gram-negative. And some of the symptoms that are described in typhus are just more like this general cloudy-inadequate state, and not like a spasm in a specific part of the brain.At the same time (not researched yet, but as clues):
- They write about it that it is an «intracellular parasite», meaning that it is embedded in the cells of blood vessels. It is like an intermediate link between viruses and bacteria. And now attention clings to the word «parasite» — tk. about the notorious eosinophilic cationic protein, first of all, they write that it increases with parasites. Well xs, is there anything in common in terms of immunity and the like, but the coincidence is powerful.
- About 3 years ago I noticed that I had a headache after monosodium glutamate. Well, it hurts and hurts, I stopped eating it, and okay. And what do we see now in rickettsia? … «Glutamate serves as a source of energy in extracellular rickettsia.» I don’t know how much it is connected either, but there are too many coincidences.
- Who knows, who knows, maybe the presence of such garbage in vascular cells led to bloody sweat that year? …
Now where can I get it from. It is transmitted in a transmissible way, that is, by all sorts of bloodsuckers. And this is where ticks come into play. I don’t know how many, but as a child I had ticks, maybe 3-10, I don’t know for sure. And ticks were never given for analysis. And I didn’t drink antibiotics. Okay, there may be no encephalitis in *** ***, but other diseases are hzkhz. The likelihood that the ticks were at least somehow sick is clearly far from zero (especially since when both my brother and I grabbed ticks in 2018, both ticks had some kind of disease).
And okay, these 3-10 ticks. My cat probably had & gt; 50 ticks. Well, they were and were, it would seem. But I remember exactly one moment in my childhood, when very evil fleas bred in her (the cat), and I remember the moment when I myself felt these fleas as they bit me. This is also a plus for the probabilities.
I admit that I don’t have specific rickettsias, but something very close in essence. Or rickettsiae, but of a separate type (not the same one that causes typhus). And there is more or less an explanation why they are relatively unexplored — these are very small bacteria. Plus, the same Lyme disease (tick-borne borreliosis) was also identified quite recently, in 1975.
Like this.
I have already passed one analysis for rickettsia — they said no. But firstly, perhaps this analysis is tailored for a specific type of rickettsia, and secondly, perhaps it works with a more acute course. And thirdly, yes, maybe these are not rickettsia themselves, but something very similar.Now I think how and where to take a piece of my vertebral arteries (from the neck) for examination under a microscope …
… (a joke with some joke …)The only thing that does not fit into the picture yet is that they write that rickettsia are very sensitive to antibiotics, incl. doxycycline. And in 2018 (after that tick) I just used horse doses of antibiotics (and doxycycline). But maybe it depends on the stage (in general, the same as with borreliosis).
And about the «lines of thought» (endothelial dysfunction and endotoxins) — this is in addition to ECP. Thinking from the other side can be said.I understand that this may turn out to be garbage, that there may be unnoticed joining, etc. I already had so many theories that I no longer regard the new ones as the only true ones, in which I am 100% sure. But so far I do not see any obvious contradictions. And even if some doctor says that all this is bullshit — again, this is not such a well-studied area (if borreliosis was found not so long ago), so the doctor may not even know ..
Collaborative research proposal
*Please note that this section was translated by Google Translatе.*
If you are a student of medical university, researcher, etc., and you are interested in the topic described in the article, it is possible to conduct joint research.
For example, to confirm / refute the version of the presence of a bacterium close to rickettsia, you can use laboratory mice — «infect» with my blood and, after a few months, examine their vessels. The result is, of course, not guaranteed.
Open to other research options.
If you are interested, email me at mbrain16@outlook.com.
About the author
At the age of 24 (2010-2011) I started to notice different transient neurological disorders varying from decrease in speech clarity to inability to perform simple mental work. Since then, I’ve visited a large number of doctors of different specializations, but the reason for the disorders remained unknown. Multiple studies did not show any pathology, and all the analyzes I was proposed to do showed values within the normal range.
The problem persisted, reducing the quality of my life and threatening my career. I continued to look for the cause myself, based on personal observations (on medical assays background), experiments with drugs and on a number of scientific articles. This article is the result of my research.
I realize that the conjecture about the role of eosinophil cationic protein may be erroneous, but I believe that it’s worth to be verified. In any case, I believe that my material may be useful for neurologists, neurophysiologists and other specialists.
Any questions and comments may be sent to mbrain16@outlook.com.
